Cancer's Hidden Weapon? Experts Reveal Diet Secrets to Boost Treatment
In recent years, the intersection of nutrition and oncology has emerged as a critical focus, sparking widespread discussion among patients, caregivers, and medical professionals. As cancer treatments become more advanced, understanding the precise roles of dietary components like sugar, protein, and "superfoods" is paramount. This article delves into the evolving scientific consensus, offering clarity on how strategic eating can support patients undergoing cancer therapy across major medical centers globally.
Background: The Evolving Landscape of Oncology Nutrition
For decades, nutritional advice for cancer patients often remained generalized, focusing primarily on maintaining weight and caloric intake. However, the late 20th and early 21st centuries ushered in an era of heightened scrutiny regarding specific macronutrients and micronutrients. The "sugar feeds cancer" hypothesis, popularized in the early 2000s, ignited a passionate debate, leading many patients to drastically alter their diets without clear medical guidance.
This period also saw a surge in interest in high-protein diets to combat cachexia, a severe wasting syndrome common in advanced cancer. Simultaneously, the concept of "superfoods"—foods purported to offer exceptional health benefits due to their nutrient density or specific compounds—gained significant traction. While some claims were rooted in preliminary laboratory studies, robust clinical evidence in human cancer patients was frequently lacking, creating a complex landscape of hope and misinformation.
Major oncology organizations, including the National Cancer Institute (NCI) and the American Cancer Society (ACS), began to invest more resources into nutritional research. Their aim was to provide evidence-based recommendations and counteract pervasive myths, shifting the paradigm from general dietary advice to more personalized, scientifically backed strategies.
Key Developments: Unpacking Modern Dietary Recommendations
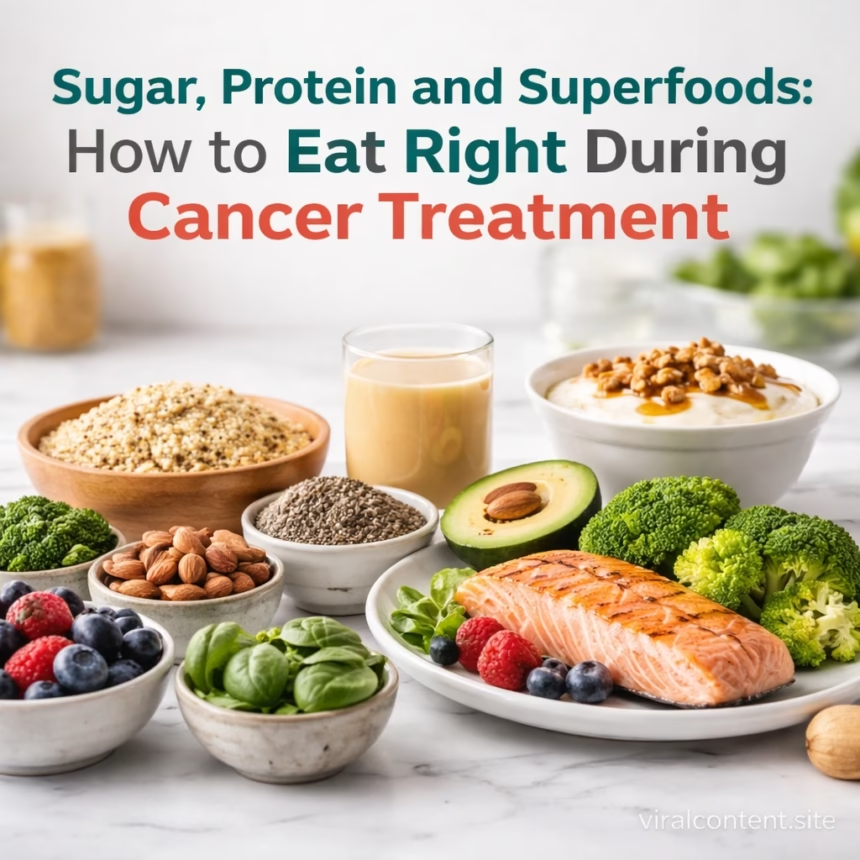
Recent years have witnessed significant strides in refining nutritional guidelines for cancer patients, moving beyond simplistic doctrines to embrace a more nuanced, evidence-based approach. Medical consensus now emphasizes a balanced, whole-foods diet tailored to individual patient needs and treatment protocols.
Demystifying Sugar’s Role
The notion that sugar directly “feeds” cancer cells and should be completely eliminated has largely been clarified by major oncology bodies. While cancer cells utilize glucose for energy, just like all other cells, completely eliminating sugar from the diet is not only impractical but potentially dangerous. Severe dietary restrictions can lead to malnutrition, weight loss, and reduced tolerance to treatment.
Current advice focuses on limiting added sugars and refined carbohydrates, which contribute to inflammation and can lead to unhealthy weight gain, rather than natural sugars found in fruits and vegetables. The emphasis is on maintaining a healthy weight and ensuring adequate caloric intake to prevent cachexia, a far greater threat to patient outcomes.
The Power of Protein for Recovery
The critical role of protein during cancer treatment has been unequivocally reinforced. Protein is essential for tissue repair, immune function, and maintaining muscle mass. Patients undergoing chemotherapy, radiation, or surgery often experience increased protein requirements due to cellular damage and inflammation.
Inadequate protein intake can exacerbate muscle wasting (sarcopenia), weaken the immune system, and delay recovery. Oncological dietitians frequently recommend higher protein intake, often ranging from 1.0 to 1.5 grams per kilogram of body weight per day, depending on the patient’s condition and treatment phase. Sources include lean meats, poultry, fish, eggs, dairy, legumes, and plant-based protein powders when whole food intake is insufficient.
Evaluating Superfood Claims
The scientific community has approached “superfoods” with cautious optimism. While many plant-based foods are rich in vitamins, minerals, antioxidants, and phytochemicals that support overall health, attributing cancer-curing properties to specific foods like blueberries, turmeric, or kale is largely unsupported by clinical trials in humans.
The focus has shifted from individual “miracle foods” to incorporating a wide variety of nutrient-dense fruits, vegetables, and whole grains into the diet. For instance, curcumin in turmeric shows promising anti-inflammatory properties in lab studies, but its bioavailability and efficacy in human cancer treatment remain under active investigation. Patients are advised to discuss any significant dietary changes or the use of high-dose supplements derived from superfoods with their oncology team, as some compounds can interact negatively with chemotherapy or radiation.
Impact: Empowering Patients and Guiding Healthcare
The refined understanding of nutrition during cancer treatment has profound implications for patients, caregivers, and the healthcare system. Clear, evidence-based guidelines empower individuals to make informed dietary choices, reducing anxiety often associated with conflicting information.
Patient Empowerment Through Knowledge
Patients are now better equipped to differentiate between scientific facts and popular myths, leading to more realistic expectations and sustainable dietary practices. This knowledge contributes to improved quality of life, better management of treatment side effects like nausea and fatigue, and enhanced physical resilience. For example, understanding that adequate protein intake can combat muscle loss can motivate patients to prioritize protein-rich foods, directly impacting their strength and ability to tolerate therapy.
Supporting Caregivers and Clinicians
Caregivers, often at the forefront of meal preparation and dietary support, benefit immensely from unambiguous guidance. They can provide nourishing meals with confidence, knowing they are contributing positively to the patient’s recovery. For healthcare providers—oncologists, nurses, and especially registered dietitians specializing in oncology—these developments provide robust frameworks for counseling.
Leading institutions like the MD Anderson Cancer Center in Houston, Texas, and the Memorial Sloan Kettering Cancer Center in New York City have expanded their nutrition departments, integrating personalized dietary assessments and interventions as standard components of cancer care plans since the mid-2010s.
What Next: The Future of Oncology Nutrition
The field of oncology nutrition is dynamic, with ongoing research promising even more precise and personalized recommendations in the coming years. Several key milestones are anticipated.
Further large-scale clinical trials are crucial to validate the efficacy of specific dietary patterns or isolated nutrients in diverse cancer populations. These studies will move beyond observational data to provide definitive evidence on how diet impacts treatment response, recurrence rates, and overall survival. For instance, trials investigating ketogenic diets in conjunction with certain chemotherapies, or specific micronutrient interventions, are currently underway at various research centers globally, including institutions in Europe and Asia.
The integration of nutritional counseling into standard oncology care is expected to become even more pervasive. This will involve routine screening for nutritional risk, early intervention by specialized dietitians, and continuous monitoring throughout the treatment journey. Digital health platforms and artificial intelligence are also poised to play a significant role, offering personalized dietary recommendations based on individual genetic profiles, microbiome analysis, cancer type, and real-time treatment side effects. This shift towards highly individualized nutrition plans represents a major step forward, moving away from a one-size-fits-all approach.
Public awareness campaigns, spearheaded by national health organizations, will continue to be vital in disseminating accurate, evidence-based information. These efforts aim to empower patients and the general public, ensuring that nutritional decisions during cancer treatment are guided by science, not by fads or misinformation. Regular updates to national and international nutritional guidelines, reflecting the latest scientific breakthroughs, will ensure that medical practice remains at the forefront of patient care.